menu
- Home
- Firm
- Practice Areas
- Automobile Accidents
- Business Litigation
- Catastrophic Injury
- Medical Malpractice
- Professional Malpractice
- Sexual Assault and Rape
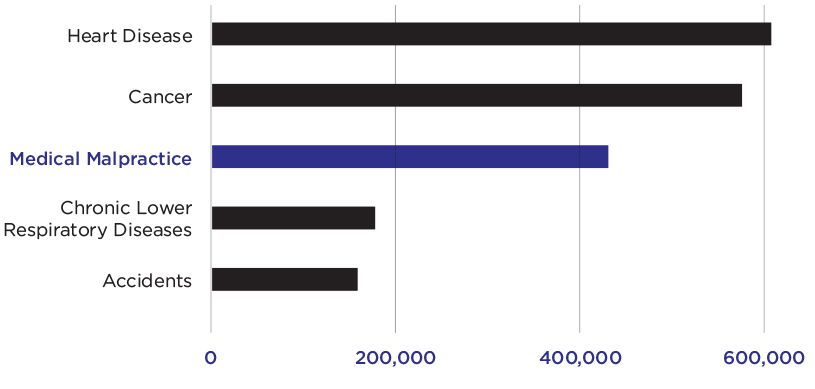
- Medical Malpractice
- Results
- Resources
- En Español
- Contact Us